Hypercholesterolaemia
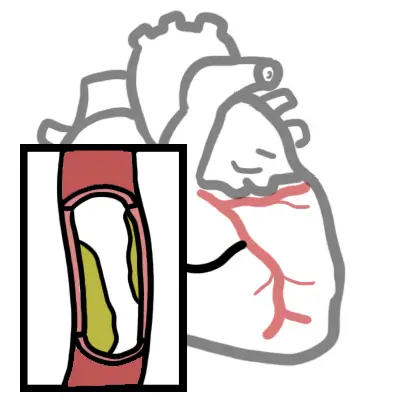
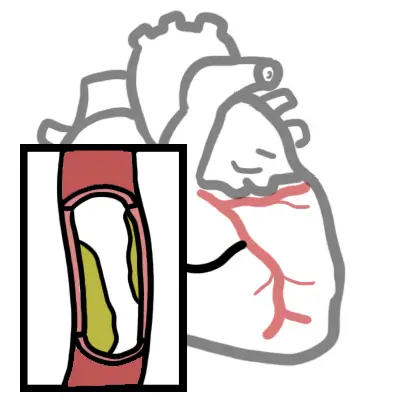
Higher levels of cholesterol associated with worse CV outcomes. Three main types that are measured: VLDL, LDL and HDL. High LDL is associated with a significant increase in cardiovascular problems. Hypercholesterolaemia can also run in families. Lifestyle modification aim to reduce cardiovascular risk. Pharmacological agents are lipid lowering drugs, statins being first-line.
Lipid Physiology
Four main lipoproteins in our body and their general function:
Chylomicrons: Assembled in mucosal epithelial cells in small intestine. Required for transport of dietary lipids to adipose tissue for storage. Made up predominately of triglycerides.
VLDL: Transports triglycerides made in hepatocytes to adipocytes for storage. Converted to LDL after depositing triglycerides. Contains predominately triglycerides
LDL: Carry about 75% of total cholesterol in blood and delivers to cell membranes and synthesis of steroid hormones and bile salts. Contains apo B100 which binds LDL receptors allowing endocytosis and breaking down to serve cellular needs. There is negative feedback inhibiting synthesis of new LDL receptors once cell has sufficient cholesterol. Predominately made up of cholesterol.
HDL: Made in the liver and removes excess cholesterol from body cells and blood and delivers to liver for elimination. Contains 40-45% protein, 30% phospholipid, 20% cholesterol, 5-10% triglyceride.
Aetiology
Hyperlipidaemia is considered to be the presence of an abnormal lipid profile, typically involving predominant hyperglyceridaemia, hypercholesterolaemia or a mixed pattern of both. It is commonly attributed to primary causes or due to high fat diet and sedentary lifestyle, however other secondary causes need consideration.
Primary (affecting lipid metabolism directly)
Secondary dyslipidaemia
Risk Factors
Clinical Examination
The following parameters are assessed:
Only the total cholesterol and high-density lipoprotein cholesterol (HDL-C) levels are required to calculate absolute CVD risk. Not LDL like one would think.
| Normal ranges for plasma lipid levels | |
| Total Cholesterol | 4.0-6.5 mmol/L |
| LDL cholesterol | <4.1 mmol/L |
| HDL cholesterol | 0.8 – 2.0 mmol/L |
| Triglycerides | 0.8-2.0 mmol/L |
| Target plasma lipid levels for patients on lipid-modifying therapy | |
| Total cholesterol | <4.0 mmol/L |
| LDL cholesterol | <2.0 mmol/L |
| HDL cholesterol | >1.0 mmol/L |
| Triglycerides | <2.0 mmol/L |
Non-pharmacological (Life-style modicfication)
Follow up every 12 months
Most effective strategy to increase HDL cholesterol levels is to reduce weight and exercise.
Pharmacological
Adverse effects of lipid-modifying therapy include liver dysfunction and muscle problems. Alanine aminotransferase [ALT] and creatine kinase [CK] should be tested at baseline and when the response of lipids is assessed (1 to 2 months after initiation or dosage adjustment).
Statins is a competitive HMG-CoA reductase inhibitor, an enzyme responsible for producing cholesterol. By lowering the levels, they help prevent heart attacks and stroke. Side effects: Headache, difficulty sleeping, flushing of the skin, myalgia, liver enzyme dysfunction, nausea or vomiting, abdominal cramping or pain, bloating or gas and serious cases myositis and Rhabdomyolysis.
Ezetimbe inhibits absorption of cholesterol at brush border of small intestine via NPC1L1 transporter. Reduces cholesterol delivery to liver, reduces hepatic cholesterol stores and increases clearance of cholesterol. Side effects: Fatigue, diarrhoea, hepatic dysfunction, arthralgia, URTI, sinusitis, influenza.
Non-pharmacological
Pharmacological
In the elderly, statin therapy has weak evidence due to the natural increase in cardiovascular risk with age, as well as adverse effects which contribute to morbidity and mortality. In general, statin therapy should be discontinued or exempted when there is no clinical benefit of treatment or risks are greater than any potential benefit.
| CARDIOVASCULAR RISK FACTORS | |
| Modifiable | Non-modifiable |
| Smoking | Increasing age |
| Hypertension | Male sex |
| Dyslipidaemia (↑Cholesterol) | Family history |
| Diabetes mellitus | Ethnicity |
| Obesity | |
| Physical inactivity | |
| High calorie intake diet | |
| Psychological stress | |
Cardiovascular risk assessment should be performed every 2 years for ≥45 year olds who do not have cardiovascular disease and are not determined to be at high risk (diabetes or with microalbuminuria, moderate or severe CKD, SBP ≥180mmHg/DBP ≥110mmHg, total cholesterol ≥7.5).
Familial hypercholesterolaemia is a dominantly inherited condition that affects over 1 in 500 people and accelerates cardiovascular disease by 20 to 40 years.
It should be considered in patients with severely elevated LDL, or those with tendon xanthomata or a strong family history of premature cardiovascular events.
UpToDate
BestPractice

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion