Remember
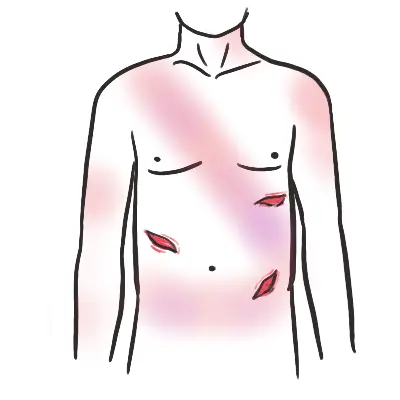
Wounds require tetanus prophylaxis and broad spectrum antibiotic if significant risk of contamination, or debridement of necrotic tissue.
History
- Likely foreign body
- Which eye
- Mechanism
- Velocity
- Protective eye wear?
- Previous eye trauma – reduced structural integrity
- When did it happen?
- Contact lens wearer
- What are the symptoms?
- Photophobia
- Discharge and type
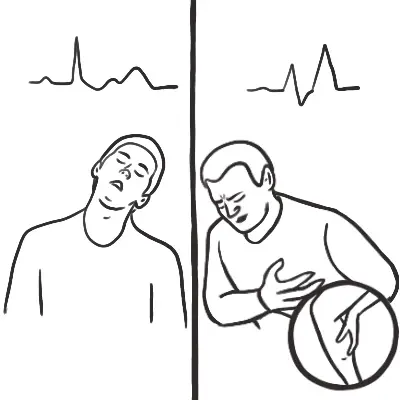
| Side note Small projectiles at high velocities increase the likelihood of penetrating trauma. Symptoms include loss of vision, pain on movement and diplopia. |
| Features requiring urgent referral |
| Contact lens wearer |
| Previous eye surgery or refractive surgery |
| Decreased vision |
| Severe pain |
| Nausea and vomiting |
| Cloudy or opaque cornea |
| Dendritic ulcer |
| Hypopyon (pus in the anterior chamber) |
| Nonreactive pupils or RAPD |
| Ocular trauma |
| Persisting or worsening symptoms |
| Chemical to eye |
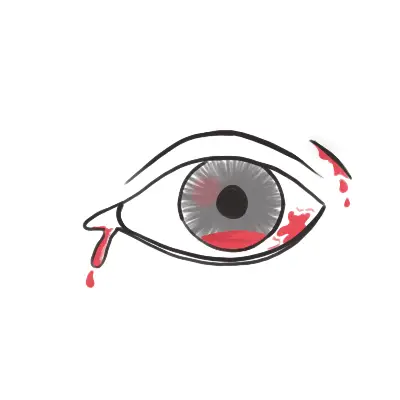
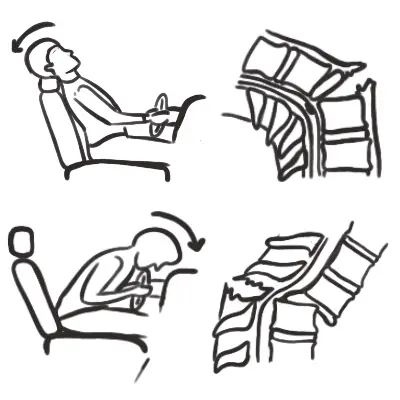
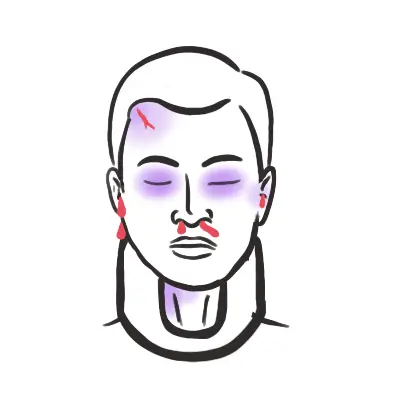
Blunt trauma
- Types
- Closed globe injury
- Ruptured globe
- Signs
- Haemorrhage
- Hyphaema
- Vitreous
- Retina → retinal detachment
- Vision changes
- Iris damage
- Lens damaged or dislocated
- Angle of eye drainage damage
- Haemorrhage
- Investigate: CT scan for orbital wall fracture
- Management: Topical antibiotics and suture eye lid lacerations and urgent referral
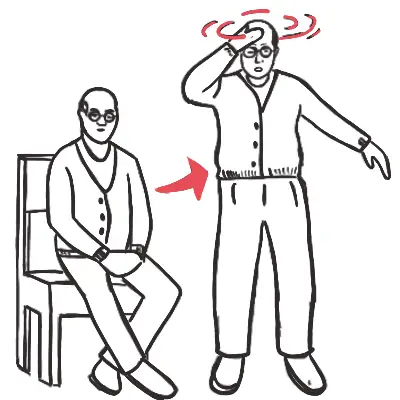
| Signs of an inferior blowout fracture |
| Ecchymosis/oedema |
| Diplopia |
| A recessed eye |
| Defective eye movement |
| Ipsilateral nose bleed |
| Diminished sensation over the distribution of the infraorbital nerve |
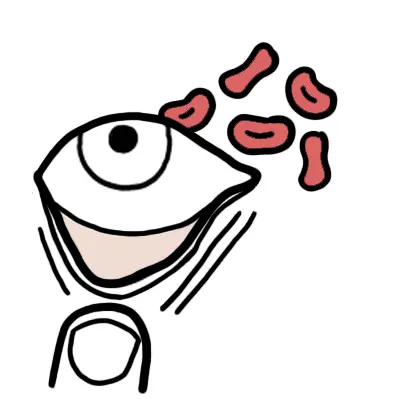
Penetrating trauma
- Prolapse of the intraocular contents and irreversible damage can occur
- Signs:
- Distorted pupil
- Cataract
- Prolapsed black uveal tissue on the ocular surface
- Vitreous haemorrhage
- Dilate pupil and search for intraocular foreign body
- Radiograph with eye in up and down gaze
- Apply shield and transfer to eye department
- All penetrating eye injuries need immediate referral
- Management:
- Nil by mouth
- Strict bed rest
- Analgesia/antiemetic
- CT
- Shield (not pad)
- Tetanus status
- Broad spectrum antibiotics
Corneal foreign body
- Any foreign body penetration of the cornea or retained foreign body will require urgent referral to ophthalmologist – immediate consult by phone
- Management removing corneal foreign body
- Topical anaesthetic
- Slit lamp and remove body
- Cotton bud
- Fine needle
- Motorised dental burr
- Use fluorescein to assess and measure the size of epithelial defect
- Topical antibiotics and cycloplegic agent
- Refer to ophthalmologist if body not removed and symptoms worsen
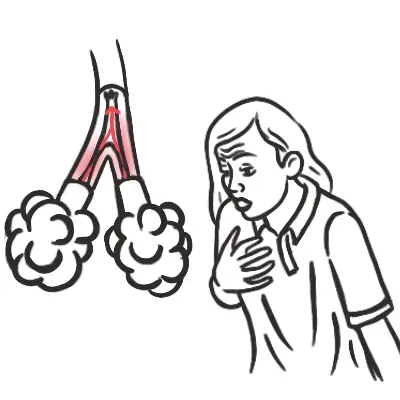
Chemical Burns Management
- Instil local anaesthetic drops to affected eye/eyes.
- Commence irrigation with 1 litre of a neutral solution, eg N/Saline (0.9%), Hartmann’s.
- Evert the eyelid and clear the eye of any debris / foreign body that may be present by sweeping the conjunctival fornices with a moistened cotton bud.
- Continue to irrigate, aiming for a continuous irrigation with giving set regulator fully open.
- If using a Morgan Lens, carefully insert the device now.
- Review the patient’s pain level every 10 minutes and instil another drop of local anaesthetic as required.
- After one litre of irrigation, review.
- If using a Morgan Lens, remove the device prior to review.
- Wait 5 minutes after ceasing the irrigation luid then check pH. Acceptable pH range 6.5-8.5.
- Consult with the senior medical oficer and recommence irrigation if necessary.
- Severe burns will usually require continuous irrigation for at least 30 minutes
- Immediate referral
| Alkali | Acidic |
| Lime | Toilet cleaner |
| Mortor & plaster | Car battery fluid |
| Drain cleaner | Pool cleaner |
| Oven cleaner | |
| Ammonia |









Discussion