Overview
Peptic ulcer refers to an ulcer in the lower oesophagus, stomach or duodenum. Incidence ↑ with age; both sexes are similarly affected. In the developed world, Helicobacter pylori incidence has been slowly ↓ over the past 50 yrs; Non-Steroidal Anti-Inflammatory drug (NSAID) use has ↑. Peptic ulcers remain common worldwide, especially in the developing world where H. pylori infection is prevalent.
| Definitions Dyspepsia: “indigestion”; describes symptoms such as bloating & nausea, thought to originate from the upper GIT; a chronic or recurrent abdominal pain or discomfort centered in the upper abdomen Ulcer: breach/ defect in mucosal lining of the stomach or duodenum that extends through the muscularis mucosae into the submucosa or deeper Erosions: breech in epithelium of the mucosa only; do not penetrate muscularis mucosae Metaplasia: a change in phenotype of differentiated cells in which one cell type is replaced by another cell type; may result in reduced functions or increased propensity for malignant transformation. |
Anatomy and Physiology
The stomach is a J-shaped organ located inferior to the diaphragm within the abdominal cavity. Stomach has three main function:
- Mixes food producing Chyme which is transferred to the dudoenum
- Secreting gastric juice
- Reservoir for food
The lower esophageal sphincter and pyloric sphincter separates the stomach from the oesophagus and duodenum respectively. The parts of the stomach include:
- Cardia – entrance from oesophagus into the stomach
- Fundus – upper portion of the stomach
- Body
- Antrum – exit of the stomach into the duodenum
Layers of the stomach
- Mucosa (most inner layer)
- Submucosa
- Muscularis Externa (3 layers inner → outer)
- Oblique
- Circular
- Longitudinal
- Serosa
The inside of the stomach looks tortuous (Rugae) and forms gastric pits which contain many cells.
The stomach have a number of specialised cells that perform varies function
- Parietal Cells → HCl (Acid) and intrinsic factor
- Chief cells → Pepsinogen
- G-cells → Gastrin
- D-cells → Somatostatin
- Enterochromaffin cells → Histamine
- Post Parasympathetic Neurons → stimulates digestion
| Remember Intrinsic factor is needed for Vitamin B12 absorption. |
Risk Factors
- H. pylori
- NSAIDs
- Smoking
- >Age
- History of peptic ulcer
- Family History of peptic ulcer
- Alcohol
- Patient in ICU on mechanical ventilation or with coagulopathy
- Chronic obstructive lung disease
- Chronic renal insufficiency
Signs and Symptoms
Clinical Presentation
- Epigastric pain +/- radiates to back (severe)
- Pain occurs shortly after eating with gastric ulcers and 2-3 hrs afterward with duodenal ulcers
- Nocturnal pain
- Pain relieved by drinking milk
- Nausea and vomiting
| Remember 3 notable characteristics: localization to the epigastrium, relationship to food, episodic occurrence. |
Examination
- Epigastric tenderness – may occur on palpation of the abdomen. But often there are no other signs on examination.
- ‘Pointing sign’ – the patient can generally show site of pain with one finger
Medical Emergency – Perforated Ulcer
- Sudden, severe abdominal pain
- Haematemesis/or melaena,
- Signs of peritonitis
- Signs of shock and anaemia
Differential Diagnosis
- Oesophageal Cancer
- Gastric Cancer
- GORD/GERD
- Gallstone Disease
- Acute Pancreatitis
- Coeliac Disease
- Irritable Bowel Syndrome
- Pericarditis
- Lower lobe Pneumonia
- Achalasia
Investigations
- H.pylori breath test or stool antigen test
- Upper Gastro endoscopy
- FBC
- Fasting serum gastrin level – hypergastrinaemia in Zollinger-Ellison syndrome
- Abdominal X-ray
- Abdominal CT
Aetiology
- Infection by H. pylori (common)
- Use of aspirin or other NSAIDs (common)
- Gastric ischaemia (‘stress ulcers’ in pts with multi-organ failure in ICUs)
- Zollinger-Ellison syndrome (gastric acid hypersecretion caused by a gastrin secreting neuro-endocrine tumour)
- Medications (potassium chloride, bisphosphonates)
- Infections & Crohn’s disease.
| Side note H. Pylori infection has reduced. This result in ↓ duodenal ulcers (almost always assoc with H. pylori infection) and ↑ in gastric ulcers (main site of ulcers caused by NSAIDs). |
Pathophysiology
Peptic ulcers result from an imbalance between factors:
- Promoting mucosal damage
- Gastric acid
- Pepsin
- Bile salts refluxed from the duodenum
- H. pylori infection
- NSAIDs)
- Promoting gastro-duodenal defense
- Prostaglandins, mucus
- Bicarbonate
- Mucosal blood flow
- Integrity of tight junctions between epithelial cells
- Restitution (process where any break in epithelium is rapidly filled by adjacent epithelial → mucosal stromal cells migrating → flattening to fill the gap).
Management
Management
- Relieve symptoms
- Induce healing
- Prevent recurrence
Medical management (mainstay of treatment, unless complicated)
H. pylori eradication:
Cornerstone of therapy for peptic ulcers as this will prevent relapse & eliminate
need for long-term therapy in the majority of patients
Triple therapy: PPI taken with 2 antibiotics (clarithromycin, amoxycillin or
metronidazole) for 14 days
Complications and Prognosis
Complications
- Penetration
- Perforation – perforation of ulcer usually anteriorly
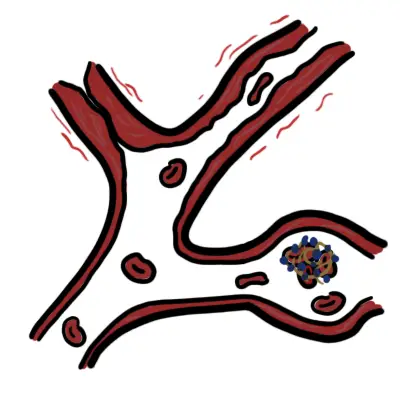
- Bleeding – ulcer erodes into the wall of a gastroduodenal blood vessel usually posteriorly
- Gastric outlet obstruction – from chronic pyloric stenosis may occur as pyloric channel ulcers heal with scarring and oedema
| Side Note Peptic ulcer penetration occurs when chronic ulcer penetrates the entire thickness of the stomach or duodenal wall, into an adjacent organ such as the pancreas, but without free perforation into the peritoneal cavity. |
Perforated Peptic Ulcer
Overview Perforated Peptic ulcer is a surgical emergency. It is caused by erosion of the ulcer through the wall of the stomach or duodenum into the peritoneal cavity. The contents of the stomach escape into the peritoneal cavity → peritonitis (board-like rigidity). The commonest site of perforation is the anterior aspect of duodenum from a duodenal ulcer.
Clinical Presentation
- Severe and sudden abdominal pain
- Signs and symptoms of Peritonitis
- Signs and Symptoms of shock
Investigation
- FBC
- EUC
- Erect Chest X-ray – reveals air under the diaphragm
- Abdo X-ray
- CT scan – indicates free intraperitoneal air
Management – Surgical Emergency
- Resuscitation
- IV Analgesia
- Surgery – of a perforated duodenal ulcer is either simple closure or a definitive procedure to decrease gastric acidity.

















Discussion