Overview
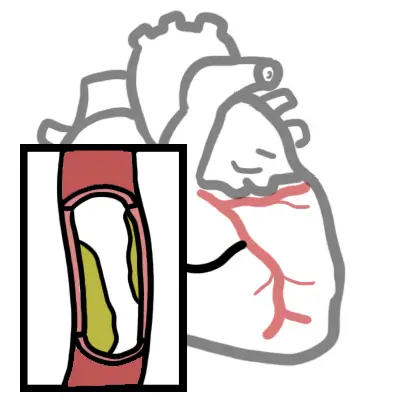
Overview Coronary artery obstruction or rupture can result in a variety of ischaemic condition which fall under the term of acute coronary syndrome. This does not include stable angina. Ischaemic heart disease is the leading cause of death world wide. The mortality of myocardial infarction is believed to be 45% with 70% of these deaths occurring before reaching medical care. It is important to reopen the artery and re-establish flow as soon as possible. This may be achieved by:
- percutaneous coronary intervention (PCI) - transluminal coronary balloon angioplasty and stenting
- fibrinolytic therapy
| Definitions Acute myocardial Infarction: Death of myocardial tissue because of inadequate blood flow ST- segment elevation myocardial infarction (STEMI): MI as defined as in acute myocardial infarction, with ST-segment elevation more than 0.1 mV in two or more contiguous leads, and elevated cardiac biomarkers. Non-ST segment elevation myocardial infarction (NSTEMI): MI, but without ST-segment elevation. May have other ECG changes, such as ST-segment depression or T-wave inversion. Will have elevated cardiac biomarkers. Unstable angina is defined by the absence of biochemical evidence of myocardial damage. It is characterised by specific clinical findings of prolonged (>20 minutes) angina at rest; new onset of severe angina; angina that is increasing in frequency, longer in duration, or lower in threshold; or angina that occurs after a recent episode of MI. |
| Remember Stable Angina is not part of Acute Coronary syndrome |
Risk Factors
| Modifiable | Non-modifiable |
| Smoking | Increasing age |
| Hypertension | Male sex |
| Dyslipidaemia | Family history |
| Diabetes mellitus | Ethnicity |
| Obesity | |
| Physical inactivity | |
| High calorie intake diet | |
| Psychological stress |
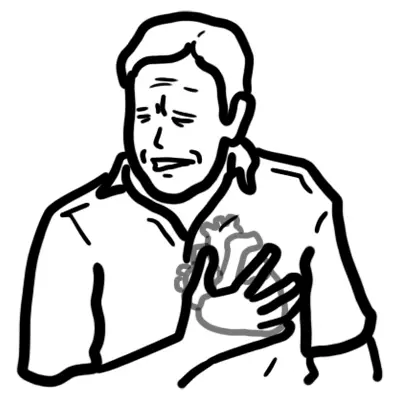
Signs and Symptoms
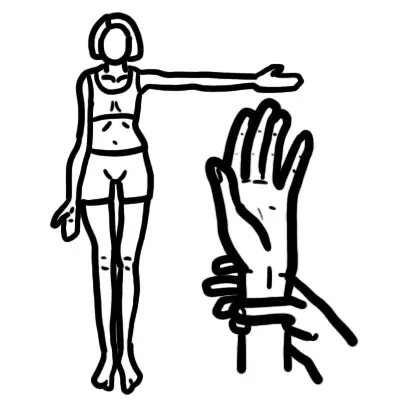
Clinical Presentation Retrosternal Pain (for at least 30min), which radiates to the neck, arms and jaw. The pain is described as crushing, heaviness or like a tight band. Worse with physical or emotional exertion. Not relieved by rest. Nitrate spray (within a couple of minutes) may not always relieve the pain. Acute coronary syndrome may be accompanied with diaphoresis, feeling of impending doom and breathless.
| Remember Patients classically clinch their fist and hold it on their chest to describe the pain (Levine's Sign) |
| Think If patient has stable angina, with rest the pain will go |
Examination
Signs of impaired myocardium
- Hypotension, Oligouria
- Raised JVP
- Narrow pulse pressure
- Third heart sound
- Lung crepitation (pulmonary edema)
Differential Diagnosis
| CAUSES OF CHEST PAIN BY BODY SYSTEMS | ||||
| Cardiac | Respiratory | Gastrointestinal | Musculoskeletal | Psychogenic |
| Acute Coronary Syndrome | Pulmonary Embolism | Oesophageal rupture | Rib Fracture | Anxiety |
| Aortic dissection | Pneumothorax | Pneumomediastinum | Herpes Zoster | Panic attack |
| Pericarditis | Pulmonary Hypertension | Cholecystitis | Costochondritis | |
| Stable Angina | Pneumonia | GERD | ||
| Endocarditis | Lung Cancer | Peptic ulcer disease | ||
| Cardiac tamponade | Bronchiectasis | Acute Pancreatitis | ||
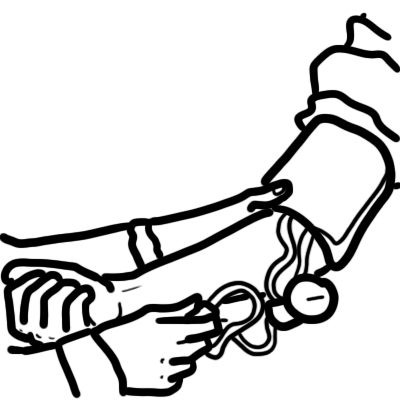
Investigation
Chest pain with high suspicion of Acute Coronary syndrome (history, examination and risk factors)
- ECG - tall T-wave, ST elevation or new Left Bundle Brach Block
- FBC
- EUC
- Glucose
- Lipid profile
- Cardiac Enzymes
- Troponin T (cTNT) and Troponin (cTNl) are proteins virtually exclusive to cardiac myocytes. They are highly specific and sensitive, but are only maximally accurate after 12 hours.
- Creatinine Kinase - CK-MM, CK-BB, CK-MB
| Think Don’t be fooled by normal cardiac enzymes. A fresh MI (< 30 minutes) may not yet show elevated blood levels. |
| Remember Troponin can be released into blood when cardiac muscle is damaged by pericarditis, PE with a large clot or sepsis. Renal failure also reduces the rate of troponin excretion. |
Diagnosis (at least two of the following):
- Typical chest pain persisting for more than 30 minutes
- Typical ECG findings
- ST elevation
- Pathological Q wave
- Elevated cardiac biomarker levels.
- Troponin (peaks in 1 -2 days) lasts 2 weeks
- CK-MB - rises 4-6 hours peaks at 12 and at 2 days drops off
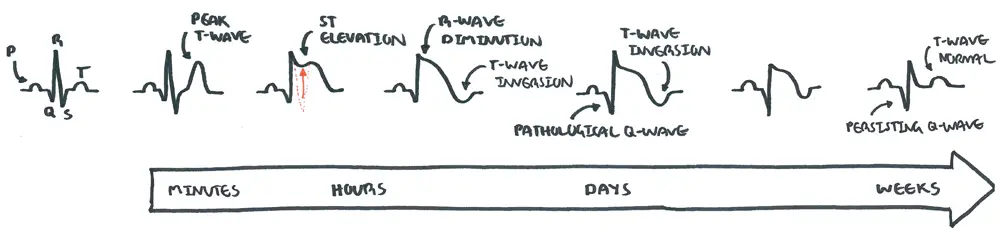
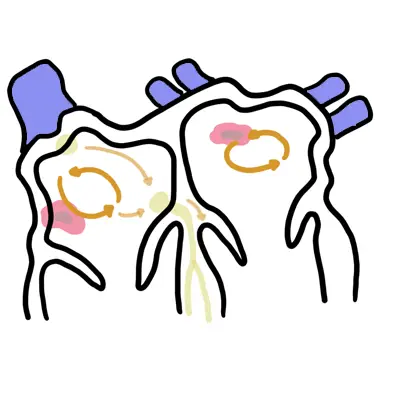
ECG
ECG is an important investigation tool for the identification and diagnosis of ACS and other cardiovascular diseases. Record ECG as soon as possible in suspected MI. Look at ST segment and look for:
- ST elevation
- ST depression
| ECG Changes in Acute Coronary Syndrome | |
| STEMI | Hyperacute T waves, which are tall, peaked, and symmetric Elevation of the ST segment (>1mm) in contiguous leads, depending upon the location of the MI. |
| NSTEMI | T wave flattening or inversion typically precedes ST segment depression Q waves are typically absent but can occur, and the duration of the ST and T wave changes is variable. |
| Unstable Angina | |
| Remember The deeper the q- wave the longer the infarction has been. |
ST Elevation Infarction of cardiac muscles results in ECG changes that evolve over hours, days and weeks in relatively predictable fashion.
Location of myocardial infarction can be identified with the ECG leads.
| Location of Infarct | ST elevation in leads |
| Anterior | V2-V5 |
| Antero-lateral | I, aVL, V5, V6 |
| Inferior | III, aVF (sometimes II also) |
| Posterior | |
| Right ventricular |
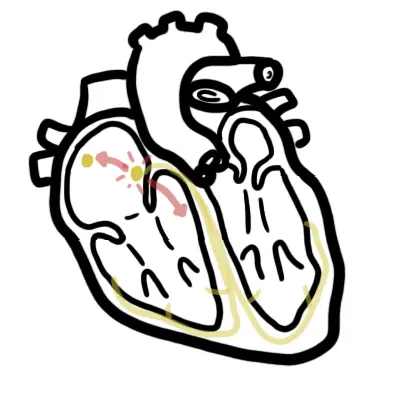
Pathophysiology
| Video: Cardiogenic Shock |
| Symptoms and signs | Mechanisms |
|---|---|
| Severe myocardial ischaemia: | |
| Chest pain | Ischaemia |
| Fourth heart sound | Forceful filling of non-compliant left ventricle |
| Low grade fever | Inflammation |
| Leucocytosis and increased levels of inflammatory markers | Inflammation |
| Increase in troponin levels | Leakage of protein from injured cardiac myocytes |
| Activation of autonomic nervous system: | |
| Tachycardia and sweating | Sympathetic activation |
| Bradycardia, nausea, and vomiting | Vagal activation (especially in inferior acute myocardial infarction) |
Source: BMJ Clinical Review Acute Coronary Syndrome 2015
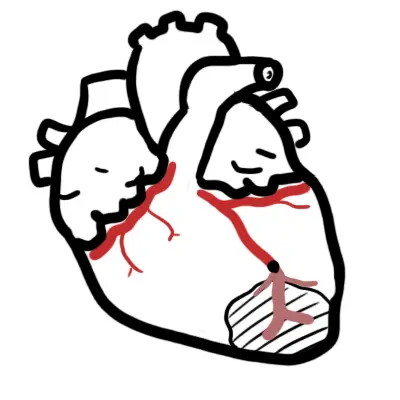
Pathology
Type of infarct
Transmural
- Affects all of the myocardial wall
- ST elevation and Q waves
Subendocardial
- Necrosis of <50% of the myocardial wall
- ST depression
| Think An ST-segment elevation on ECG indicates that the infarction extends through the full thickness of the myocardial wall (transmural). The absence of ST-segment elevation in the setting of cardiac enzymes indicates that the infarction is limited to the subendocardium. NSTEMIs are dangerous in that the patient is still at risk for a full-thickness infarct in that area. |
| PATHOLOGICAL CHANGES | ||
| Time from onset | Gross Findings | Microscopic Findings |
| 1-3 hours | Pallor of mycocardium | No inflammatory cells |
| 4-12 hours | Coagulation necrosis, inflammation (oedema, oesoinophil and neutrophil infiltration) | |
| <24 hours | Coagulation necrosis | Coagulation necrosis |
| 1-3 days | Central area of yellow discoloration surrounded by a thin rim of highly vascularized hyperemia | Macrophage infiltration |
| 3-7 days | Fibroblast infiltration | |
| Days 7 - 21 | ||
Management STEMI
| Definition PCI: Percutaneous coronary intervention (angioplasty and/or stenting). Thrombolytics: Drugs such as tissue plasminogen activator (tPA), streptokinase, and reteplase (r-PA), which act to lyse fibrin thrombi in order to restore patency of the coronary artery when PCI is contraindicated or is not available |
Must consider the following in managing ACS:
- The suspicion of acute MI based on the clinical and ECG findings
- Deciding whether the patient has indications or contraindications for thrombolytics or primary percutaneous coronary intervention
- Excluding other diagnoses that might mimic acute MI but would not benefit from or might be worsened by anticoagulation or thrombolysis (eg, acute pericarditis, aortic dissection).
Acute management
- Admission to coronary care unit
- Explain to patient what has happened
- Morphine
- Oxygen
- Nitrates
- Aspirin
- Clopidogrel
- Acute management Reperfusion therapy
- Percutaneous coronary intervention (PCI) OR Fibrinolytic therapy (thrombolysis)
| Remember MONAC Morphine (+/- antiemetic), Oxygen, Nitrates, Aspirin, Clopidogrel |
Acute management Reperfusion therapy
Early reperfusion with PCI or thrombolytics reduces mortality and preserves ventricular function in patients who have ST-segment elevation, have no contraindications, and receive treatment within the first 6 to 12 hours
- PCI should be performed within:
- 60min if patient presents within the first hour of symptom onset
- 90min if patient presents between 1-3hrs after symptom onset
- 90 to 120 minutes for patients presenting between 3 and 12 hours
- If these targets cannot be reached, fibrinolysis should be given within 30 minutes of arrival in hospital
- Fibrinolytic therapy (Thrombolysis) within 24 hours, contraindication >24hours
- Alteplase OR
- Reteplase
- Anticoagulant therapy
- Hepain
- Heart Bypass
| Indications for reperfusion therapy |
| Ischaemic/infarction symptoms of longer than 20 minutes (chest pain-radiating to shoulder or jaw, sweating, feeling of doom |
| Symptoms commenced within 12 hours |
| ST elevation or presumed new left bundle branch block on ECG |
| No contraindications to reperfusion therapy. |
| Pharmacology Thrombolytics break down/dissolve clots. It is used to treat stroke, pulmonary embolism and myocardial infarction. Three main thrombolytic drugs: tissue plasminogen activator, streptokinase, andurokinase. Side effects: major bleeding, cardiac arrhythmias, cholesterol embolus syndrome, anaphylactoid reaction, cerebrovascular accident, intracraneal hemorrhage. Steptokinase specific adverse effects: Non-cardiogenic pulmonary edema, hypotension, fever and shivering. |
| Contraindication and cautions for thrombolysis use in STEMI |
| Risk of Bleeding (active bleeding, haemorrhage ophthalmic condition, known bleeding diathesis, suspected aortic dissection) |
| Risk of intracranial haemorrhage |
| Recent Major trauma, surgery, head injury <3weeks |
| Aortic Dissection |
| Pregnancy |
On-going management Non-pharmacological
- Smoking cessation
- Alcohol limitation
- Diet modification
- Lose weight
On-going management pharmacological (ABAS)
- ACE inhibitors OR Angiotensin Receptor Blocker
- Beta-blockers
- Aspirin + clopidogrel
- Statins
Long-term anticoagulation to prevent emboli from left ventricular mural thrombus should be considered in patients who have suffered a large myocardial infarction, particularly if a large akinetic/dyskinetic area is present.
| Pharmacology Aspirin is a COX 1/2 inhibitor. It prevents the production of Prostagladins (inflammation: fever and pain) and thromboxane (clotting). It is used to treat fever, osteoarthritis, heart conditions and stroke. Side effects: nausea/vomiting, dyspepsia, stomach ulcer or bleeding problems, headache, dizziness, tinnitus, renal dysfunction and Reye’s syndrome (particularly in children who have taken aspirin) |
Complication and Prognosis
Complication
- Arrythmia
- Myocardial Rupture
- Shock/CHF
- Post-Infart Angina
- Recurrent MI
- Thromboembolism/PE
- Pericarditis
- Dressler's Syndrome
| Dressler's Syndrome This is a type of pericarditis that can develops 2-10 weeks after an MI, heart surgery (or even pacemaker insertion). |
Prognosis Factors associated with poor prognosis
- Age >70
- Previous MI or chronic angina
- Anterior MI or right ventricular infarction
- LV failure at presentation
- Hypotension at presentation
- Diabetes Mellitus
- Acute Mitral regurgitation
- Ventricular septal defect